NUHS Institutions will NEVER ask you to transfer money or disclose bank details over a call.
If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
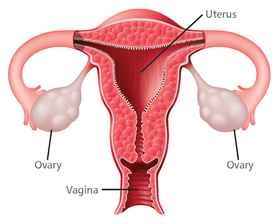
The ovaries are part of a woman’s reproductive system. They are located in the pelvis. Each ovary is the size of an almond. The ovaries make the female hormones – estrogen and progesterone. They also release eggs. An egg travels from an ovary through a fallopian tube to the womb (uterus). When a woman goes through her menopause, her ovaries stop releasing eggs, resulting in far lower levels of hormones being produced. The ovaries contain primitive cells, which are cells that go on to become eggs, and epithelial cells. Primitive cells that become cancerous are called germ cell tumours. Epithelial cell cancers of the ovary are more common than germ cell cancers.
Ovarian cancer is the 5th most common cancer in Singaporean women. It’s incidence is increasing in Singapore. Ovarian cancer is known as the deadliest gynaecological cancer because it is usually detected in its later stages of development and spread. The main reason for this is that the ovaries are located deep in the body cavity and hidden away in this manner, pre-cancerous and early cancerous changes are not only difficult to medically detect but also are not obvious or apparent to the women with these early changes.
The CA125 blood test and other related tumor marker blood tests are NOT effective screening tests for ovarian cancer. Regular ultrasounds of the ovaries in normal healthy women with no obvious family history of ovarian, breast or colon cancers are also NOT effective in screening for ovarian cancer. These tests are often offered as part of routine health screening packages and may help to pick up other non-cancerous conditions, but are NOT effective in detecting ovarian cancer in the general population. If you are in good general health and your mother, her sisters or your sisters have never had ovarian, breast or colon cancer, inform your healthcare provider that you would like to decline the CA125 blood test.
The most effective early detection tool against ovarian cancer is YOU, armed with the knowledge of early symptoms, being aware of your own body and having regular pelvic examinations by your gynaecologist.
*People who think they may be at risk should discuss this with their doctor.
Unfortunately, early ovarian cancer often does not cause obvious symptoms. This is why it is often known as a "silent killer". But, as the cancer grows, symptoms may include:
Most often these symptoms can also be caused by problems other than cancer, only a doctor can tell for sure. Any woman with these symptoms should consult her doctor right away.
If you have a symptom that suggests ovarian cancer, your doctor must find out whether it is due to cancer or to some other cause. Your doctor may ask about your personal and family medical history.
You may have one or more of the following tests.
Physical Exam
Your doctor checks general signs of health. Your doctor may press on your abdomen to check for tumours or an abnormal build-up of fluid. A sample of fluid can be taken to look for ovarian cancer cells.
Pelvic Exam
Your doctor feels the ovaries and nearby organs for lumps or other changes in their shape or size.
Blood Tests
Your doctor may order blood tests. The lab may check the level of several substances, including CA-125. CA-125 is a substance found on the surface of ovarian cancer cells and on some normal tissues. A high CA-125 level could be a sign of cancer or other conditions. The CA-125 test is not used alone to diagnose ovarian cancer. This test is approved by the Food and Drug Administration for monitoring a woman's response to ovarian cancer treatment and for detecting its return after treatment.
Ultrasound
The ultrasound device uses sound waves that people cannot hear. The device aims sound waves at organs inside the pelvis. The waves bounce off the organs. A computer creates a picture from the echoes. The picture may show an ovarian tumour. For a better view of the ovaries, the device may be inserted into the vagina (transvaginal ultrasound).
Biopsy
A biopsy is the removal of tissue or fluid to look for cancer cells. Based on the results of the blood tests and ultrasound, your doctor may suggest surgery (a laparotomy) to remove tissue and fluid from the pelvis and abdomen. Surgery is usually needed to diagnose ovarian cancer.
Laparoscopy
The doctor inserts a thin, lighted tube (a laparoscope) through a small incision in the abdomen. Laparoscopy may be used to remove a small, benign cyst or an early ovarian cancer. It may also be used to learn whether cancer has spread.
For ovarian cancer, most women have surgery and chemotherapy.
Surgery
The surgeon makes a long cut in the wall of the abdomen. This type of surgery is called a laparotomy. If ovarian cancer is found, the surgeon removes:
If the cancer has spread, the surgeon removes as much cancer as possible. This is called "debulking" surgery.
If you have early Stage I ovarian cancer, the extent of surgery may depend on whether you want to get pregnant and have children. Some women with very early ovarian cancer may decide with their doctor to have only one ovary, one fallopian tube, and the omentum removed.
Chemotherapy
Chemotherapy uses anticancer drugs to kill cancer cells. Most women have chemotherapy for ovarian cancer after surgery. Some women have chemotherapy before surgery. Chemotherapy is given in cycles. Each treatment period is followed by a rest period. The length of the rest period and the number of cycles depend on the anticancer drugs used. You may have your treatment in a clinic, at the doctor's office. Some women may need to stay in the hospital during treatment.
Cancer is a complex condition and knowledge about cancer and cancer treatment is constantly changing and getting more sophisticated to deliver ever better patient outcomes. The very best cancer care is therefore best delivered by a team of professionals, with each member of the team being an expert in their own field but working TOGETHER to take care of the whole person.
At the NCIS, we believe that when we treat the WHOLE PERSON, a WHOLE PERSON walks out our doors. This is the philosophy and thinking that lies at the heart of our Whole Person Approach to Ovarian Cancer Care at the NCIS.
The women we care for may have ovarian cancer, but the disease is only one part of a whole person who is a living, breathing and feeling entity. At the NCIS, we believe in not only treating cancer but making people whole after their time with us, and this starts with having a team of dedicated healthcare professionals support each and every aspect of the whole person as we journey with our patients through diagnosis, treatment, recovery and beyond.
The Ovarian Cancer Journey @ NCIS
The Women’s Emotional Health Service (WEHS)
This team of emotional health specialists are an important component of the ovarian cancer care solution. Quite simply, a fit emotional state ensures a healthy immune system that fights cancer more effectively. Effective emotional assessment and support is a complex, constantly evolving process and something the Women’s Emotional Health team does exceptionally well, supporting a growing community of healthy, happy ovarian cancer survivors, one woman at a time. Our patients are supported through a combination of CARE therapy, hypnotherapy and medical therapeutics. At the NCIS, we are proud of the important work that our WEHS team does, and our cancer survivors agree!
Dietetics and Cancer Nutrition
At the NCIS, we believe that fueling the whole person is an important first step in winning the fight against ovarian cancer. Most ovarian cancer patients will experience a loss of weight and appetite which makes getting nutrition back on track a critical first thing to do in caring for women living with ovarian cancer. Our nutrition and dietetics team helps support our patients through their cancer care journey by formulating diet plans, adjusting supplementary nutrition through treatment and recovery and are adept at managing advanced nutritional support for our sickest women.
The Total Lymphoedema Team
Lymphoedema is a complex and potentially debilitating condition that develops as a result of cancer surgery and therapy in some patients. At the NCIS, we believe that the best treatment is prevention. This belief is embodied in the creation of the Total Lymphoedema Clinic (TLC) to support all the women living with cancer that we care for at the NCIS who may be at risk for lymphoedema. The team at the TLC consists of surgeons, physicians, physiotherapists, nurses and occupational therapists who are all committed to one thing, helping our patients come out of ovarian cancer care WHOLE and functional with sub-specialty professionalism and Tender Loving Care.
Advanced Practice and Specialty Nursing
At the NCIS, we love our nurses for one very simple reason. Our Advanced Practice and Specialty nurses translate all the expertise available at NUH in to the care that our patients receive. The women living with ovarian cancer that walk in our doors walk out whole because of the dedication and professionalism that these cancer professionals show all day, every day. Effective cancer care is an incredibly complex process which our Advanced Practice and Specialty nursing team has the training, education and expertise to understand, coordinate and help deliver to the women receiving care for ovarian cancer at the NCIS. It’s no wonder that our cancer survivors hug a cancer specialty nurse wherever they meet one!
The Ovarian Cancer Treatment Team at NCIS is spearheaded by Professor Jeffrey Low accompanied by his team of medical professionals.
The team is committed to delivering uncompromised and dedicated clinical research, expertise and care in the prevention, management and cure of Ovarian Cancer.
Gynaecologic Oncology
Medical Oncology
Pathology
Radiation Oncology
Radiology