Radiation therapy is a crucial component of cancer treatment and here at the NCIS, the Radiation Therapy Centre (RTC) is committed to providing our patients with excellence in radiation therapy treatments.
We aim to deliver the best care for our patients through the following:
Our radiation treatments are tailored to individual patients' unique circumstances with reference to international guidelines such as those published by the National Comprehensive Cancer Network (NCCN). This emphasis on adhering to established international benchmarks is aligned with our commitment to achieve high-quality treatment across the board for our patients.
Our diverse team of radiation oncologists works within sub-specialty teams focusing on specific tumour groups. This enhances expertise development and allows for incorporation of the latest advancements into our treatment protocols.
Our sub-specialty teams work closely with our surgical and medical oncology colleagues to deliver coordinated patient care. Discussions of complex oncological conditions led by the expertise of relevant specialists are facilitated by our multi-disciplinary tumour boards.
The Department of Radiation Oncology is committed to delivering quality treatments safely. Multiple layers of process checks are put in place by our team of dosimetrists, medical physicists and audit team to maximise safety. This includes peer-review of all our radiation treatment plans.
During radiation therapy treatment, image-guidance through cone beam CT imaging or electronic portal imaging is done to confirm accuracy of patient set-up before the radiation is delivered.
We offer a comprehensive range of radiation therapy services tailored to each individual patient's needs, including both external beam and brachytherapy modalities.
Delivery of successful radiation therapy requires the coordinated efforts of a dedicated team of staff with different skill sets.
Our Radiation Oncology Team comprises:
Radiation Oncologists
Radiation oncologists are medical specialists who are qualified to give radiation therapy. The radiation oncologist’s role is to determine the suitability of radiation therapy for each patient, and to give the final approval for the radiation therapy plan. During the course of treatment, the radiation oncologist is also responsible for reviewing patients for side effects. After treatment is completed, the radiation oncologist determines the frequency of follow-up and subsequent tests.
Our radiation oncologists are also actively engaged in undergraduate and post-graduate teaching, as well as clinical research.
Head of Department
SENIOR CONSULTANT
CONSULTANT
ASSOCIATE CONSULTANT
RESIDENT PHYSICIAN/REGISTRAR/CLINICAL ASSOCIATE
Dr Lee Chia Ching
Dr Katherine Meng Tian
Dr Syadwa A Shukor
Dr Sreyes Ravi
Dr Wei Wei
Dr Caryn Wujanto
Dr Ye Chen'En
Dr Yip Pui Lam
Dr Teri Danielle Yeoh
Radiation Therapists

Radiation therapists are a group of allied health professionals who are trained to operate the various systems required in the delivery of radiation therapy to our patients. These systems include data acquisition systems like CT simulation, planning systems for designing radiation therapy plans, as well as treatment units like linear accelerators that ultimately carry out the treatment.
The specific duties of Radiation Therapists include:
Radiation Therapists also play an important role in clinical research and implementation of new techniques and protocols in cancer treatment to provide holistic care to our patients.
HEAD, RADIATION THERAPY | |
|---|---|
| |
SENIOR PRINCIPAL RADIATION THERAPIST | |
|
|
PRINCIPAL RADIATION THERAPIST | |
|
|
SENIOR RADIATION THERAPIST | |
|
|
RADIATION THERAPIST | |
|
|
Medical Physicists
Medical physicists provide the scientific and technical support in a radiation oncology department. They assist in creating, implementing and monitoring the procedures which allow the best treatment using radiation, taking into account the protection and safety of patients and others involved in the treatment process.
Medical physicists make sure that all equipment meet international and national standards. This can include machines such as linear accelerators, CT scanners, treatment computer systems and radioactive materials. They are also responsible for the design of new radiation oncology facilities and the commissioning of new equipment.
Medical physicists train other professional groups on topics such as radiation physics and radiation safety. They also have both a primary and supporting role in research activities in a radiation oncology department.
CHIEF MEDICAL PHYSICIST | |
|---|---|
| |
SENIOR PRINCIPAL RADIATION PHYSICIST | |
| |
SENIOR RADIATION PHYSICIST | |
| |
RADIATION PHYSICIST | |
|
Radiation Oncology Nurses

Radiation Oncology Nurses are licensed registered nurses who work collaboratively with radiation oncologists and radiation therapists to care for patients at the time of initial consultation, during radiation treatment, and at follow-up appointments.
Our nurses provide the following important functions leading up to a patient's successful treatment:
Symptom Management and Patient Education
Prior to the initiation of radiation therapy, radiation oncology nurses provide counseling for patients and their caregivers on the possible side effects of treatment they may experience. During radiation therapy, they will assess patients for ongoing toxicity and advise them on appropriate nursing care. Where necessary, they may also actively manage the symptoms, for instance, applying necessary dressing to skin affected by radiation therapy.
Assistance in Medical Procedures
Sometimes, radiation therapy may involve specialised procedures requiring placement of applicators, sedation or clinical monitoring. In these instances, our nurses are often called upon to assist the radiation Oncologist to ensure the procedures are done effectively and safely.
Emotional Support
Recognising that the period of radiation therapy can be a difficult time for patients and their loved ones, our nurses are available to provide support and counseling. They can help patients access various community resources and support groups, as well as assist with issues such as home care, hospice or medical equipment.
Patient Care Associates and Patient Service Associates

Patient Care Associates (PCAs) and Patient Service Associates (PSAs) are ancillary staff who play key roles in the coordination of patient care and general administration.
They are responsible for the registration of patients upon arrival, handling of appointments and assisting the doctor during consultation. When a decision is made for radiation therapy, they will provide the necessary financial counseling before treatment is initiated. Our PCAs and PSAs work closely with the different teams in the Radiation Therapy Centre to help create a better experience for our patients.
PATIENT SERVICE COORDINATOR | |
|---|---|
| |
SENIOR PATIENT SERVICE ASSOCIATE | |
| |
PATIENT SERVICE ASSOCIATE | |
|
|
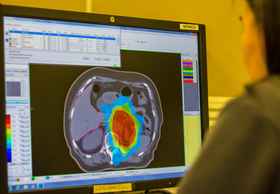
IMRT allows for (red cloud) to be effectively delivered to the tumour (green line) while sparing the adjacent kidney.
Intensity Modulated Radiation Therapy (IMRT) / Volumetric Modulated Arc Therapy (VMAT)
Intensity Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) use sophisticated computer algorithms paired with dynamic multi-leaf collimators (MLCs) to deliver high doses of radiation to tumours while sparing nearby critical organs. Volumetric Modulated Arc Therapy (VMAT) offers potentially shortened treatment times by integrating movements of the treatment gantry with movements of the dynamic MLCs. Currently, these techniques are utilised in head & neck cancers, prostate cancer, and other tumour sites where radiation therapy needs to be delivered to relatively large areas, yet require sparing of nearby organs.
New services available at NCIS@RTC include:
|
HyperArc® 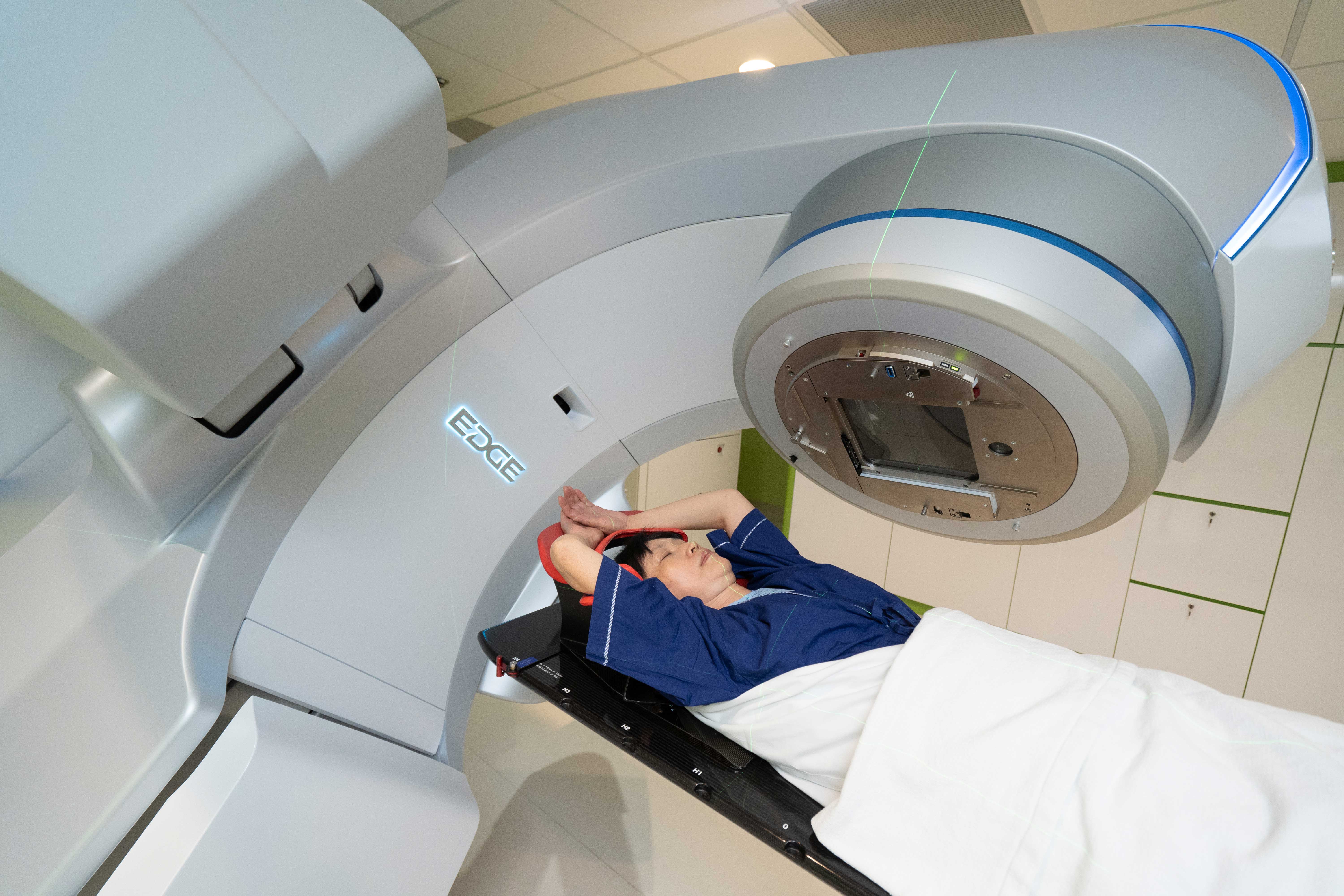 Stereotactic radiosurgery/radiotherapy for benign and malignant brain tumours has demonstrated durable tumour control and symptomatic relief with acceptable toxicity in suitable patients. HyperArc® high-definition radiotherapy from Varian was designed and optimised for intracranial central nervous system radiosurgery applications. In addition to fast treatment delivery, HyperArc® can highly conformal X-ray dose distributions to the multiple brain lesions with steep dose gradients, which has the potential to spare the adjacent normal structures and to improve the accuracy of patient set-up and target localisation. |
|
Proton Therapy It is a type of particle therapy that uses a beam of protons to irradiate tumours. The chief advantage of proton therapy over other types of external beam radiotherapy is that the dose of radiation is deposited over a narrow range of depth; this can result in less exit or scattered dose to surrounding healthy tissues. we will assess the suitability and benefit for proton therapy against traditional radiotherapy. Where appropriate, we will provide access for patients to receive proton therapy |
|
Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiation Therapy (SBRT) 
Immobilisation via a whole body vacuum bag to achieve positioning required for stereotactic radiotherapy. These specialised treatment techniques make use of precise positioning, immobilisation devices and multiple treatment beams to achieve highly focused radiation therapy targeting tumours. This allows larger radiation doses to be delivered during each treatment, thereby shortening the treatment duration without compromising safety. SRS is typically used for tumours in the brain. SBRT (also known as stereotactic ablative radiotherapy) can be used to treat small tumours in the lung, liver, spine or other organs. In certain tumour sites like the lung and liver, respiratory motion may compromise the therapeutic efficacy of stereotactic techniques. For such cases, respiration control capabilities are available including Active Breath Control (ABC) which limits such motion, as well as 4D CT simulation that can account for tumour motion at the planning stage. |
|
High Dose Rate (HDR) Brachytherapy 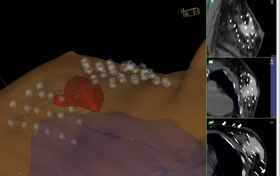
3D reconstruction and planning for breast brachytherapy High Dose Rate (HDR) Brachytherapy is able to deliver extremely high doses of radiation therapy to tumours with minimal normal tissue effects through the use of Iridium-192 sources placed directly at the tumour site through the use of specialised applicators. HDR Brachytherapy is used in gynaecological tumours such as cervical and uterine cancers, as well as prostate and breast cancer treatments. For cervical cancer, HDR brachytherapy is a critical component of successful treatment by allowing the safe delivery of curative doses of radiotherapy to the tumour. For prostate cancer, HDR brachytherapy can be used either as a standalone treatment or in conjunction with external beam radiation therapy, and hence can shorten the overall treatment duration. Selected breast cancer cases can also be treated with HDR brachytherapy, which will allow radiation treatment to be shortened to just one week instead of three to six weeks. At NCIS, each brachytherapy treatment is planned with the benefit of full 3D imaging through CT simulation, allowing us to know the exact dose delivered to the tumour and the nearby normal organs. |
|
3D Conformal Radiation Therapy 
Patient being prepared before radiation therapy treatment 3D Conformal Radiation Therapy makes use of 3-dimensional imaging and computer-based planning to deliver radiation therapy to targeted areas while sparing normal organs. Its versatility and proven track record makes it a suitable and reliable radiation therapy technique for almost all tumour sites. |
|
Electron Therapy 
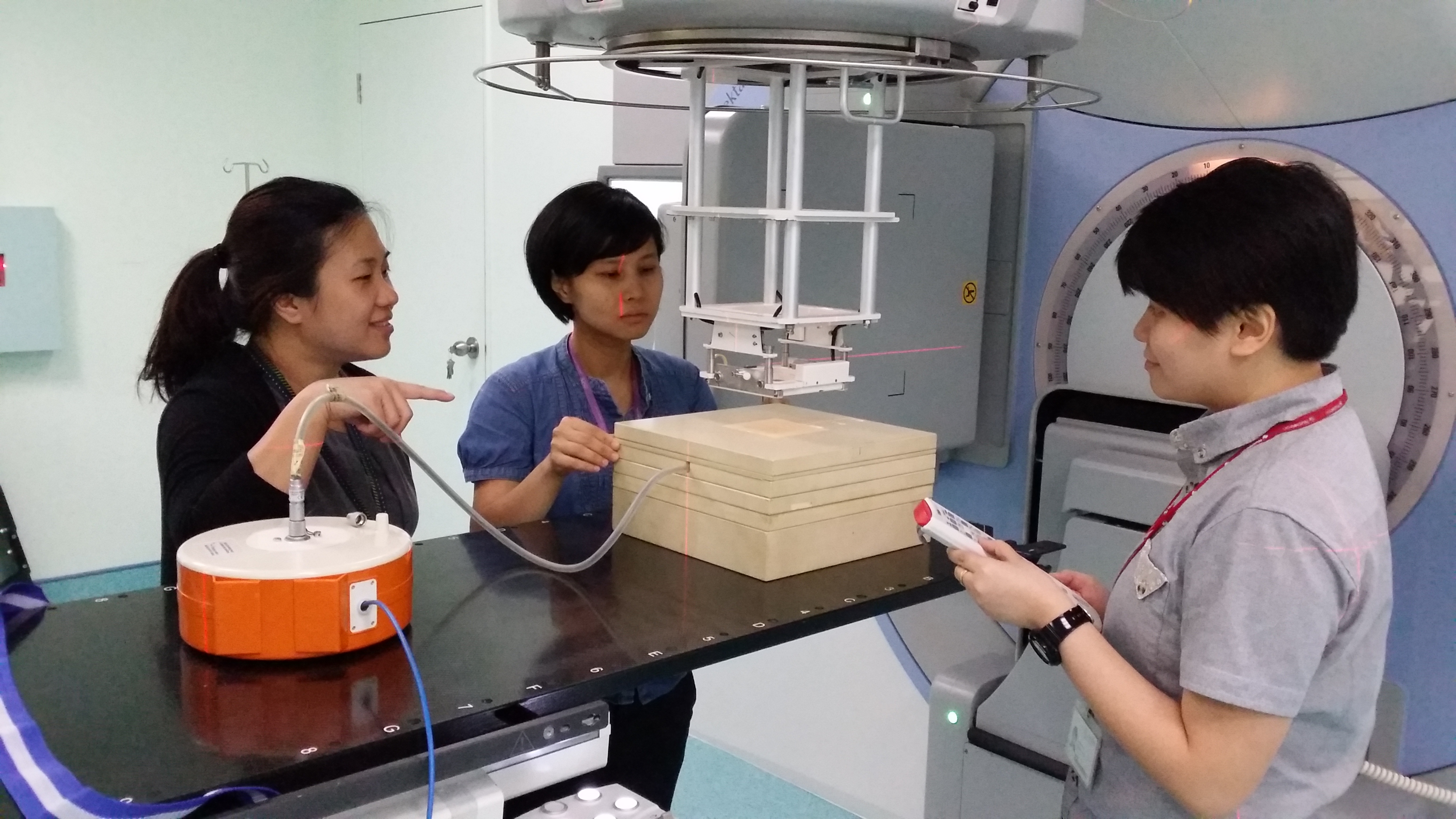
Radiation therapists using laser lights and light fields to verify setup before delivering electron therapy Electron Therapy allows for the radiation dose to be deposited at the skin surface while sparing deep, normal tissues. This property of electrons makes it suitable for the treatment of skin and other superficial tumours. We can tailor the electron energies to target tumours of varying depths. |
|
Image-Guided Radiation Therapy (IGRT) 
Cone beam CT evaluation for positional accuracy immediately prior to radiation therapy treatment Image guidance can be used with any external beam technique to optimise patient positioning immediately prior to initiating radiation therapy. We often use cone beam computed tomography (CT) to visualise the body’s internal structures in three dimensions. These near real-time images enable us to make fine positional adjustments, ensuring that radiation therapy is delivered to the intended tumour location precisely, while sparing normal organs. Cone beam CT imaging is a marked improvement over traditional imaging methods which are limited by their two-dimensional nature and lower resolution images. |
First-timer? Not to fret, let us walk you through the process of what to expect during your visit at our Radiation Therapy Centre.

During consultation, your radiation oncologist will explain the need for radiation therapy and the potential side effects. Step 1 - Consultation When you are first referred for a radiation oncology review, you will be seen by a radiation oncologist who will discuss with you the need for radiation therapy for your condition, and the potential side effects that you may encounter. Sometimes, further tests may be required before a decision to embark on radiation therapy can be made. Do not hesitate to ask your oncologist if you have queries about how the treatments are administered, the duration of the treatments, potential side effects and how these will be minimised and managed, as well as alternatives to radiation therapy treatments. If a decision to administer radiation therapy is reached, you will be given financial counselling on treatment charges, subsidies and the quantum of eligible Medisave and Medishield deductions. Before you leave, you will also be given appointment dates for CT simulation as well as the commencement date of your radiation therapy. |

CT simulation staff guiding patient on optimal position Step 2 - CT Simulation During CT Simulation, a CT scan will be done on the area that requires treatment. This scan is done in the treatment position, and may require the use of immobilisation devices. In addition, small permanent reference marks may be placed on the body. The immobilisation devices and reference marks enable us to reproduce the position accurately during treatment, which is crucial for successful treatment. As far as possible, your therapists will ensure that the scan and treatment position is comfortable for you. Do let them know if you face any discomfort or are unable to maintain the required position. For certain treatments, you may be required to have a full bladder or empty stomach. If contrast is needed for the scan, an intravenous plug will be placed for administration of contrast. Please inform us if you have any kidney problems, asthma or previous allergies to contrast. Typically, a CT Simulation will require between 30 to 60 minutes. It may take slightly longer if the treatment is expected to be complex, requiring specialised equipment or preparatory work beforehand. |
Radiation oncologist and therapist reviewing the plan before final approval. Step 3 - Planning After the CT simulation is done, the images are exported to a treatment planning system software. Thereafter, the radiation oncologist will identify the tumour and the areas at risk that require radiation therapy, as well as the critical organs that should be avoided. Next, our radiation therapists with specialised skills in planning will work closely with the radiation oncologists to design a radiation therapy plan that best delivers radiation to the tumour while minimising the dose to normal tissues and organs. This process is important in achieving the best possible outcome for our patients and requires adequate time. Often, a few rounds of optimisation are required before the best plan is selected. After the plan is finalised, it undergoes several layers of checks to ensure optimal treatment, safety and accuracy of the delivered plan. |

A significant portion of daily treatment time is spent to place the patient in the exact treatment position required Step 4 - Treatment and Review When the radiation therapy sessions commence, you will be required to attend treatment daily. A radiation therapy schedule will be provided to you to inform you of your treatment times. During treatment, radiation therapists will position you exactly as you were during the CT Simulation. You will undergo radiation therapy in a treatment room with radiation therapists monitoring your progress via a CCTV during the process. Some days, treatments may seem to last longer due to additional imaging being done to ensure accuracy of the treatment. During the course of treatment, you will be scheduled for weekly appointments to see your radiation oncologist where you will be monitored for any side effects developed during the treatment process, as well as tumour response, if applicable. You may also be given medication to relieve some of the side effects. In addition, weekly consultations with our in-house dietitian may be arranged for patients whose nutritional status warrant review. |

A follow-up session will be conducted to monitor any potential side effects as well as track tumour response to treatment. Step 5 - Follow-Up Upon completing the course of radiation therapy, you will be given a follow-up appointment. The purpose of a follow-up session is to monitor the side effects as well as tumour response. This may sometimes involve additional imaging like diagnostic CT scans, MRI scans or blood tests. |
The Department of Radiation Oncology at NCIS has earned numerous awards and accolades for its contributions to the field of radiation oncology in Singapore. Here are some noteable achievements from the department.
Below are summaries of some recent scientific publications by our staff members.
Acute radiation dermatitis is a common side effect of radiotherapy, which is a type of cancer treatment. However, there's no universally agreed-upon way to care for patients with this condition. This is mainly because the current guidelines differ and the evidence supporting them is contradictory. To address this, an international group of 42 experts used a method called the Delphi consensus process to review existing medical literature and establish a consensus on how to manage and prevent this condition. The experts agreed on six methods for preventing acute radiation dermatitis: photobiomodulation therapy and Mepitel film for breast cancer patients, Hydrofilm, mometasone, betamethasone, and olive oil. For managing existing cases, they recommended Mepilex Lite dressings. However, most potential treatments couldn't be recommended because there wasn't enough evidence to support their effectiveness, the evidence was conflicting, or the experts couldn't reach a consensus. This suggests that more research needs to be done in this area. Until then, doctors can consider using the agreed-upon methods in their practice to help their patients deal with acute radiation dermatitis. |
This study studied the health of 2,600 Asian patients diagnosed with a type of cancer called diffuse large B-cell lymphoma (DLBCL) between 2000 and 2018. The researchers found that about 24% of these patients died from the lymphoma and about 9% developed heart-related illnesses, known as cardiovascular diseases (CVDs). Certain factors, like being older, having high blood pressure or diabetes, and using aspirin, increased the risk of developing CVDs. Particularly at-risk patients (those aged 61-75, smokers, diabetics, and those treated with a medication called doxorubicin) lived with DLBCL for around 8 years and with a CVD for around a month, due to the high risk of death once a CVD develops. The study concluded that doctors should carefully consider treatment options to minimize the risk of CVDs in DLBCL patients. |
3. State-of-the-Art Imaging Techniques in Metastatic Spinal Cord Compression. This paper provides an overview of the best imaging techniques used to diagnose Metastatic Spinal Cord Compression (MSCC), a serious complication in cancer patients. The paper discusses the pros and cons of various imaging methods, including MRI, CT scans, and CT Myelogram, and their role in planning and verifying treatments like stereotactic body radiotherapy (SBRT). MRI is considered the best method, with high accuracy. However, CT scans can be useful in emergency situations when MRI is not available. The paper also looks at how new tech, such as deep learning tools, can help detect spinal issues faster, allowing for quicker treatment and better patient outcomes. |
We reviewed and compared the effectiveness and safety of two types of radiation therapy: stereotactic body radiation therapy (SBRT) and conventional external beam radiation therapy (cEBRT). These treatments are used for patients suffering from painful bone metastases (cancer that has spread to the bones). The study found that SBRT was more effective in completely relieving pain after three months and slowing down the local progression of the cancer. However, it also led to an increase in short-term pain flare-ups. The two types of radiation therapy did not differ significantly in quality of life and overall survival. |
We explored how radiation therapy for stomach cancer, which unintentionally exposes the spleen to radiation, affects the severity of lymphopenia (a condition where you have fewer lymphocytes, a type of white blood cell, than normal). This could impact survival time and risk of infection. The study looked at patients who underwent this therapy between 2015 and 2020. Findings show that higher radiation doses to the spleen resulted in more severe lymphopenia, leading to a higher risk of infection and lower survival rates. This suggests that adjusting the radiation to lower the dose to the spleen may reduce the risk of severe lymphopenia. |
The paper investigated a phase 1 clinical trial aimed at figuring out the right dose of a combined treatment strategy for resistant ovarian cancer that does not respond to common platinum-based treatments. The trial examined a combination of weekly paclitaxel (a chemotherapy drug) and low-dose fractionated whole abdominal radiation therapy. The study involved patients who had been heavily treated before, and they found that the combo treatment was well tolerated and had encouraging results. For some patients, their cancer was controlled for a period of time and for others, their cancer tumor markers decreased by over 50%. This suggests that this treatment strategy might be worth further investigation for use in ovarian cancer that is resistant to common treatments. |
7. Palliative radiotherapy for bladder cancer: a systematic review and meta-analysis The study investigated the effects of different radiation therapy doses on symptom relief for advanced bladder cancer patients. Researchers looked at a variety of studies and focused on how well symptoms like blood in urine, painful urination, and frequent urination were managed. They found that higher doses of radiation didn't necessarily improve the relief of these symptoms. However, a higher radiation dose did seem to lengthen the time that blood in urine was controlled, and it reduced the improvement of painful urination. There was also a notable occurrence of severe side effects, affecting the digestive and urinary systems, in about a quarter of patients. The study concluded that more research is needed to understand how palliative radiation therapy affects the quality of life of patients with advanced bladder cancer. |
We explored whether using a preventive radiation technique, called prophylactic irradiation of tracts (PIT), can stop cancer from spreading along the path of a surgical incision or biopsy needle in patients with malignant pleural mesothelioma (MPM), a type of lung cancer. This study looked at several clinical trials that compared patients who received PIT with those who didn't after undergoing a chest wall procedure for MPM. The analysis found that PIT significantly reduced the risk of cancer spreading along the procedure tract. However, it didn't seem to affect overall survival rates. This suggests that PIT could be a useful strategy in preventing the spread of cancer after diagnostic or therapeutic chest wall procedure in patients with MPM. |
We examined the risk of stroke and death within a month after stroke in survivors of nasopharyngeal cancer (NPC), a type of cancer that starts in the upper part of your airway, behind the nose. The study looked at patients diagnosed with NPC over a span of around 13 years. The findings showed that survivors of NPC, particularly those diagnosed with early-stage disease, had a significantly higher risk of having a stroke compared to the general population. However, if they did have a stroke, their chances of dying within 30 days were not significantly higher. These findings suggest that doctors need to pay special attention to the potential risk of stroke in people who have survived NPC. |
The paper looked at whether radiotherapy after mastectomy (PMRT) improves outcomes for elderly patients (over 65 years old) with intermediate-risk breast cancer. The study analyzed other research published over a decade to compare the effects of PMRT with no PMRT for these patients. The researchers found that PMRT was associated with a relative reduction in the risk of death and breast cancer-related death, but the results were not conclusive. Some studies didn't show a significant difference in local and distant disease recurrence between the two groups. So, while the benefits of PMRT for this group of patients are not entirely clear, it's suggested that those with multiple risk factors indicating a high risk of local recurrence after mastectomy should consider PMRT. More research is needed to better understand which elderly patients might benefit from PMRT. |